A CLOSER LOOK
/ST. PAUL’S HOSPITAL’S OVERDOSE PREVENTION SITE
Is Our Densely Populated Neighborhood The Best Location For This Service?
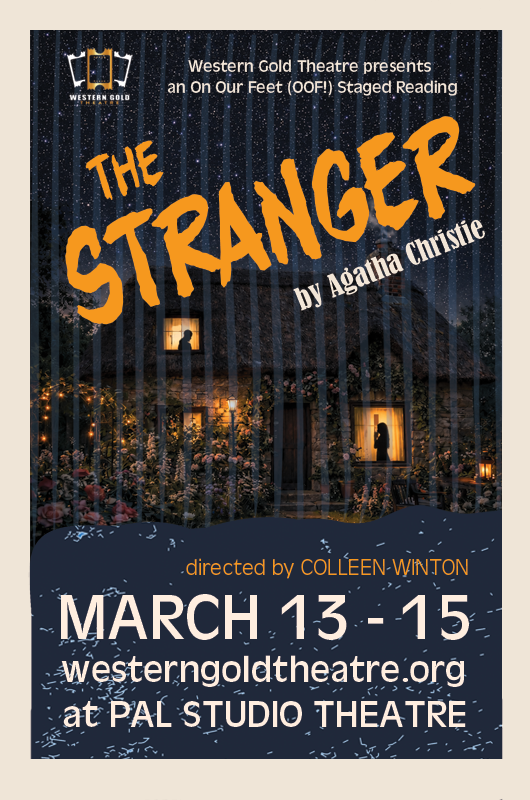
The Overdose Prevention Site trailer behind St. Paul’s Hospital at Thurlow and Comox. (Photos by John Streit)
by John Streit
Back in July of 2019, an online article by the Daily Scan via Providence Health Care celebrated the first birthday of “Canada’s first peer-led, hospital-associated” Overdose Prevention Site (OPS) at St. Paul’s Hospital in the West End. That year, the OPS was situated in a small tent in the hospital courtyard and 10,000 people were said to have visited. The Daily Scan profiled Will, a regular drug user at the tent who had spent 17 years behind bars.
Will said the conversations he had with peers at the OPS prompted his desire for treatment and recovery. “It’s such a positive environment here and the staff are so understanding,” Will said. Photos showed cake and a BBQ.
On its website, RainCity Housing, the local non-profit organization which manages the Overdose Prevention Site, describes it as “a place where a person can be safely monitored while using drugs and treated immediately if they overdose. It also offers drug testing and provides harm reduction supplies, harm reduction education, and referrals to health services, addictions services, and other social supports.” It adds, “service users are excited to be able to walk to something close to their home, where they can feel safe using.”
A tribute to murdered OPS volunteer Thomus Donaghy on the side of the St. Paul’s Hosptial Overdose Prevention Site trailer.
Fast forward to 2020 where there is growing concern among some West Enders that the OPS, now in a trailer on Comox and Thurlow across from Nelson Park, is partly contributing to an increase in neighbourhood disorder and a rise in crime. Residents on social media have been actively urging each other to be careful when walking home at night, watch for needles near the dog park and elementary school, and never lock a bike outside.
John Bishop is a former business management professional with a long connection to St. Paul’s Hospital. After retiring in 2014, he started volunteering at Positive Living B.C., then the B.C. Persons with AIDS Society. “I frequently met and networked with senior officials from the health authorities, the B.C. Centre for Disease Control and Dr. Julio Montaner of the B.C. Centre for Excellence in HIV/AIDS to advance the interests of and advocate for those living with HIV/AIDS in B.C.”
Bishop took a break for a few years then began volunteering at St. Paul’s Hospital as a greeter/ navigator at the main Burrard Street entrance.
He also happens to live right across the street from the hospital. Bishop says he and his neighbours have been front row witnesses to what has been happening near the Overdose Prevention Site. “We watched people we had never seen in our neighbourhood before begin to congregate on the steps of the old Nurses Building, inject out in the open, lean against our building huddled over their fix. Drug paraphernalia began to litter the street. Then the verbal assaults and physical threats began, targeting our friends coming to visit, residents trying to get home, trying to get in the door before being attacked.”
Bishop claims many of the drug addicts coming to the West End are also homophobic. “I’ve witnessed this in some of the programming that Positive Living had run over the years. We have witnessed this in the verbal assaults and physical threats that have been directed at us since the OPS moved to the trailer.”
With his connection to the hospital, years of volunteer work and advocacy, and in a desperate search for answers, Bishop felt comfortable reaching out to staff and volunteers at RainCity Housing. “I learned that, since the OPS went into operation over two years ago, RainCity people have been attacked and assaulted in both of the previous locations. They have been verbally threatened, attacked at knifepoint, and pepper-sprayed. They confided in me that they knew hard-core predator drug dealers from the Downtown Eastside were moving into the area, that they were actively engaged in selling drugs to the users of the OPS.” He believes management at St. Paul’s Hospital does not understand or isn’t acknowledging this.
The West End Journal reached out to Providence Health Care which owns the hospital but was told that during the election period, they were “limited in the information they can provide.” TWEJ also reached out to RainCity Housing but has yet to receive a reply.
According to Bishop’s sources at the OPS, clients are allowed to get their drugs tested and then inject them on-site or pick up clean needles and leave to inject elsewhere. “I’m told that since the death of Thomus most are now choosing to leave — too afraid to hang around,” says Bishop.
At a busy store near the OPS, the young staff were recently shaken up after witnessing two people in the throes of an overdose in the back alley. One long-time employee, who did not want his name used, says one of the OD victims appeared frozen, slowly turning blue on some stairs. A pharmacist from the store quickly administered Naloxone. “The other person was face down in a puddle. I pulled him out. Paramedics arrived and gave him several shots of Naloxone. As they took him away, stolen merchandise from our store poured onto the ground. He had been caught stealing from us the day before. Two other guys refused to stay with their friends to let the paramedics know what drugs they had taken because their Denny's meal was getting cold … seriously.”
Vancouver Police tell TWEJ that calls for service in the area of Comox and Thurlow (which includes St. Paul’s Hospital) increased from 612 in 2018 to 1,530 in 2019. Crime stat analysts say most of the calls are for disturbances and suspicious persons. So far this year, police have been called to the area 587 times, but the VPD believes that number would surpass last years’ total if not for the temporary closure of the OPS in July.
Tragically, that closure was because of the July 27 homicide of Thomus Donaghy, an overdose prevention worker at the OPS. His death hit the community hard. A memorial to Donaghy, including his image, has been spray-painted onto the side of the trailer and partly reads “a local hero, friend missed by the entire city, world…”
A man from Victoria has been charged with manslaughter and remains in custody. Five weeks later, the OPS reopened with extra security and safety protocols in place.
B.C. is almost five years into a provincial health emergency declared because of the opioid crisis. Almost six thousand people have died. Suspected drug overdose deaths skyrocketed 71 percent in August compared to the same month last year. 147 people died.
Andy Watson with the B.C. Coroners Service says there is no silver bullet to try and solve this crisis but overdose prevention sites in addition to other harm reduction, like drug checking services, are all crucially important.
“We know it’s not for everyone - it’s not a one size fits all approach. But certainly, we know that there hasn’t been a single overdose death at a supervised consumption site or OPS.” He believes what we have now is not enough. “It’s a step in the right direction and we need to look at innovative ways. If we need to be bold and courageous, then we need to do so.”
Bishop says he and his friends understand the need for an OPS.
“We have lost friends to fentanyl tainted drugs. We want to see it succeed but not at the expense of those who work and live in and around St. Paul’s. One community should not be put in harm’s way to help another community that is already in harm’s way. That only shifts the burden of safety from one agency, St. Paul’s Hospital to another, the VPD.”